Nutritional Status Correlated with Frailty Among Elderly
DOI:
https://doi.org/10.26699/jnk.v12i1.ART.p071-079Keywords:
Elderly, Frailty, Nutritional StatusAbstract
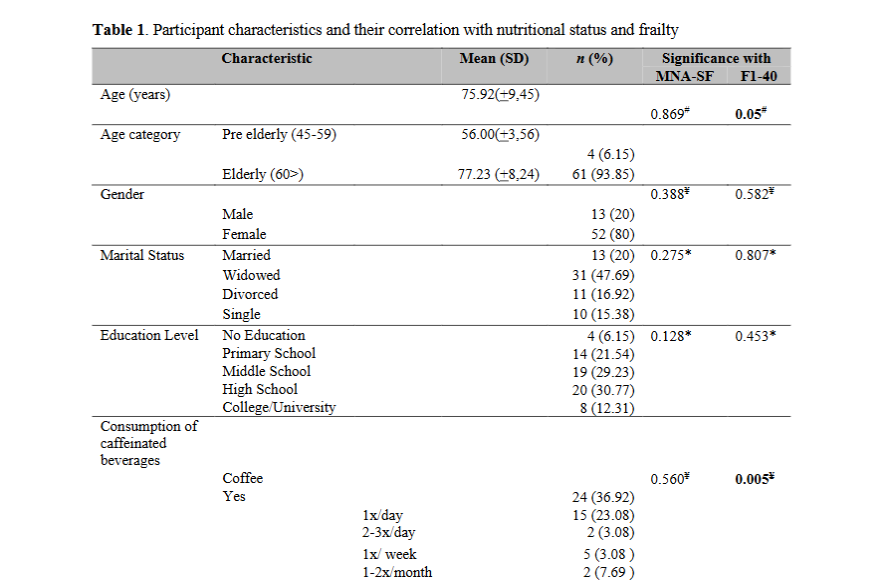
Nutritional status is a critical issue for older adults and is closely linked to various health problems. Insufficient or excessive dietary intake can impair the body’s ability to manage physical disorders and diseases, leading to increased weakness in this population. This research aimed to analyze the correlation between nutritional status and frailty in the elderly. This research utilized a cross-sectional design, employing consecutive sampling to gather data from 65 patients in four nursing homes. Participants were elderly individuals over 45 years old, residing in nursing homes, cooperatives, and willing to participate. Sample size determination was performed using G*power 3.1.9.7 software, with a medium effect size of 0.41, a p-value of 0.05, and a power of 0.90. Non-parametric tests were used for data analysis, employing the MNA-SF and Frailty Index Questionnaire-40 (FI-40) instruments. The average age of participants was 75.92 (+9.45) years, with the majority of the sample being elderly, and women constituted 80% of all participants. There was a significant correlation between nutritional status and frailty (p=0.005 <0.05), with a moderate negative relationship (r=-0.344). This research concluded that the better the nutritional status, the lower the frailty level. This research indicated that better nutritional status was linked to reduced frailty in the elderly, highlighting the need for healthcare teams to implement strategies that enhance patient adherence in managing factors that negatively affect nutrition.
References
Amelia, W. R., Leoni, A. P., Syauqy, A., Laksmi, P. W., Br Purba, M., Noer, E. R., Nofi, L. S., Sundari, B., & Arini, M. (2023). Malnutrition at Hospital Admission and Its Associated Factors in Internal Medicine Inpatients. Jurnal Gizi Indonesia (The Indonesian Journal of Nutrition), 11(2), 128–139. https://doi.org/10.14710/jgi.11.2.128-139
Badan Pusat Statistik. (2023). Statistik Penduduk Lanjut Usia. Badan Pusan Statistik, 20.
Bakhtiari, A., Pourali, M., & Omidvar, S. (2020). Nutrition Assessment and Geriatric Associated Conditions Among Community Dwelling Iranian Elderly People. BMC Geriatrics, 20(1). https://doi.org/10.1186/S12877-020-01668-8
Cahyawati, W. A. S. N., Panghiyangani, R., Muslim, M. S. A., & Rahman, N. B. (2022). Relationship between Nutritional Status, Frailty, and Cognitive Function among Elderly at Dr. H. Moch. Ansari Saleh General Hospital Banjarmasin. Jurnal Kedokteran Brawijaya. https://doi.org/10.21776/UB.JKB.2022.032.01.10
Calder, P. C. (2021). Nutrition and Immunity: Lessons for Covid-19. Nutrition & Diabetes, 11(1). https://doi.org/10.1038/S41387-021-00165-0
Chi, J., Chen, F., Zhang, J., Niu, X., Tao, H., Ruan, H., Wang, Y., & Hu, J. (2021). Impacts of Frailty On Health Care Costs Among Community-dwelling Older Adults: A Meta-analysis of Cohort Studies. Archives of Gerontology and Geriatrics, 94, 104344. https://doi.org/10.1016/J.ARCHGER.2021.104344
Cruz-Jentoft, A. J., & Woo, J. (2019). Nutritional Interventions to Prevent and Treat Frailty. Current Opinion in Clinical Nutrition and Metabolic Care, 22(3), 191–195. https://doi.org/10.1097/MCO.0000000000000556
Deschasse, G., Bloch, F., Drumez, E., Charpentier, A., Visade, F., Delecluse, C., Loggia, G., Lescure, P., Attier-Zmudka, J., Bloch, J., Gaxatte, C., Van Den Berghe, W., Puisieux, F., & Beuscart, J. B. (2022). Development of a Predictive Score for Mortality at 3 and 12 Months After Discharge From an Acute Geriatric Unit as a Trigger for Advanced Care Planning. The Journals of Gerontology: Series A, 77(8), 1665–1672. https://doi.org/10.1093/GERONA/GLAB217
Eggersdorfer, M., Berger, M. M., Calder, P. C., Gombart, A. F., Ho, E., Laviano, A., & Meydani, S. N. (2022). Perspective: Role of Micronutrients and Omega-3 Long-Chain Polyunsaturated Fatty Acids for Immune Outcomes of Relevance to Infections in Older Adults-A Narrative Review and Call for Action. Advances in Nutrition, 13 5(5), 1415–1430. https://doi.org/10.1093/ADVANCES/NMAC058
Fang, H., Tu, S., Sheng, J., & Shao, A. (2019). Depression In Sleep Disturbance: A Review On a Bidirectional Relationship, Mechanism and Treatment. Journal of Cellular and Molecular Medicine, 23(4), 2324–2332. https://doi.org/10.1111/JCMM.14170
Gielen, E., Beckwée, D., Delaere, A., De Breucker, S., Vandewoude, M., Bautmans, I., Bautmans, I., Beaudart, C., Beckwée, D., Beyer, I., Bruyère, O., De Breucker, S., De Cock, A. M., Delaere, A., De Saint-Hubert, M., De Spiegeleer, A., Gielen, E., Perkisas, S., & Vandewoude, M. (2021). Nutritional Interventions to Improve Muscle Mass, Muscle Strength, and Physical Performance in Older People: An Umbrella Review of Systematic Reviews and Meta-analyses. Nutrition Reviews, 79(2), 121–147. https://doi.org/10.1093/NUTRIT/NUAA011
Hai, S., Gao, Q., Gwee, X., Chua, D. Q. L., Yap, K. B., & Ng, T. P. (2021). Malnutrition Risk, Physical Function Decline and Disability in Middle-Aged and Older Adults Followed Up in the Singapore Longitudinal Ageing Study. Clinical Interventions in Aging, 16, 1527–1539. https://doi.org/10.2147/CIA.S322696
Hong, X., Yan, J., Xu, L., Shen, S., Zeng, X., & Chen, L. (2019). Relationship Between Nutritional Status and Frailty in Hospitalized Older Patients. Clinical Interventions in Aging, 14, 105–111. https://doi.org/10.2147/CIA.S189040
Inayah, Z., & Aini, N. (2019). Biostatistika dan Aplikasi Program.
Jamain, M., Udaya, W., Sudarso, A., Rasyid, H., Makbul Aman, A., & Seweng, A. (2020). Association between Muscle Mass with Frailty State in Elderly. Indian Journal of Public Health Research & Development, 11(6), 1310–1315. https://doi.org/10.37506/IJPHRD.V11I6.9984
Kementrian Kesehatan RI. (2023). Berhaji dan Lansia.
Kim, Y. J., & Karceski, S. (2021). Alzheimer Disease and Mood. Neurology, 97(13), 1363–1366. https://doi.org/10.1212/WNL.0000000000012607
Kirk, B., Prokopidis, K., & Duque, G. (2021). Nutrients to Mitigate Osteosarcopenia: The Role of Protein, Vitamin D and Calcium. Current Opinion in Clinical Nutrition and Metabolic Care, 24(1), 25–32. https://doi.org/10.1097/MCO.0000000000000711
Krishnamoorthy, Y., Vijayageetha, M., & Saya, G. (2021a). Validation and Reliability Assessment of The Mini-nutritional Assessment-short Form Questionnaire Among Older Adults in South India. Indian Journal of Community Medicine, 46(1), 70–74. https://doi.org/10.4103/IJCM.IJCM_208_20
Krishnamoorthy, Y., Vijayageetha, M., & Saya, G. (2021b). Validation and Reliability Assessment of the Mini-Nutritional Assessment–Short Form Questionnaire among Older Adults in South India. Indian Journal of Community Medicine : Official Publication of Indian Association of Preventive & Social Medicine, 46(1), 70–74. https://doi.org/10.4103/IJCM.IJCM_208_20
Leij-Halfwerk, S., Verwijs, M. H., van Houdt, S., Borkent, J. W., Guaitoli, P. R., Pelgrim, T., Heymans, M. W., Power, L., Visser, M., Corish, C. A., & de van der Schueren, M. A. E. (2019). Prevalence of Protein-energy Malnutrition Risk in European Older Adults In Community, Residential and Hospital Settings, According to 22 Malnutrition Screening Tools Validated for Use in Adults ≥65 Years: A Systematic Review and Meta-analysis. Maturitas, 126, 80–89. https://doi.org/10.1016/J.MATURITAS.2019.05.006
Lin, C. C., Shih, M. H., Chen, C. D., & Yeh, S. L. (2021). Effects of Adequate Dietary Protein with Whey protein, Leucine, and Vitamin D Supplementation On Sarcopenia in Older Adults: An Open-label, Parallel-group Study. Clinical Nutrition, 40(3), 1323–1329. https://doi.org/10.1016/J.CLNU.2020.08.017
Liu, W., Chen, S., Jiang, F., Zhou, C., & Tang, S. (2020). Malnutrition and Physical Frailty among Nursing Home Residents: A Cross-Sectional Study in China. The Journal of Nutrition, Health & Aging, 24(5), 500–506. https://doi.org/10.1007/S12603-020-1348-X
Maharani, A., Pendleton, N., & Leroi, I. (2019). Hearing Impairment, Loneliness, Social Isolation, and Cognitive Function: Longitudinal Analysis Using English Longitudinal Study on Ageing. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry, 27(12), 1348–1356. https://doi.org/10.1016/J.JAGP.2019.07.010
Mugica-Errazquin, I., Zarrazquin, I., Seco-Calvo, J., Gil-Goikouria, J., Rodriguez-Larrad, A., Virgala, J., Arizaga, N., Matilla-Alejos, B., Irazusta, J., & Kortajarena, M. (2021). The Nutritional Status of Long-Term Institutionalized Older Adults Is Associated with Functional Status, Physical Performance and Activity, and Frailty. Nutrients, 13(11). https://doi.org/10.3390/NU13113716
Norazman, C. W., Adznam, S. N., & Jamaluddin, R. (2020). Physical Frailty Among Urban-Living Community-Dwelling Older Adults in Malaysia. International Journal of Environmental Research and Public Health, 17(18), 1–14. https://doi.org/10.3390/IJERPH17186549
Pang, S., Miao, G., Zhou, Y., Duan, M., Bai, L., & Zhao, X. (2023). Association between coffee intake and frailty among older American adults: A population-based cross-sectional study. Frontiers in Nutrition, 10, 1075817. https://doi.org/10.3389/FNUT.2023.1075817/BIBTEX
Phua, J., Visaria, A., Østbye, T., & Malhotra, R. (2022). Association of Vision and Hearing Impairments with Quality of Life Among Older Adults: Mediation by Psychosocial Factors. Geriatrics & Gerontology International, 22(1), 56–62. https://doi.org/10.1111/GGI.14318
Rizka, A., Indrarespati, A., Dwimartutie, N., & Muhadi, M. (2021). Frailty among Older Adults Living in Nursing Homes in Indonesia: Prevalence and Associated Factors. Annals of Geriatric Medicine and Research, 25(2), 93–97. https://doi.org/10.4235/AGMR.21.0033
Rodríguez-Mañas, L., Rodríguez-Sánchez, B., Carnicero, J. A., Rueda, R., García-Garcia, F. J., Pereira, S. L., & Sulo, S. (2021). Impact of nutritional status according to GLIM criteria on the risk of incident frailty and mortality in community-dwelling older adults. Clinical Nutrition, 40(3), 1192–1198. https://doi.org/10.1016/J.CLNU.2020.07.032
Santini, Z. I., Jose, P. E., York Cornwell, E., Koyanagi, A., Nielsen, L., Hinrichsen, C., Meilstrup, C., Madsen, K. R., & Koushede, V. (2020). Social Disconnectedness, Perceived Isolation, and Symptoms of Depression and Anxiety Among Older Americans (NSHAP): A Longitudinal Mediation Analysis. The Lancet. Public Health, 5 1(1), 62–70. https://doi.org/10.1016/S2468-2667(19)30230-0
Setiati, S., Laksmi, P. W., Aryana, I. G. P. S., Sunarti, S., Widajanti, N., Dwipa, L., Seto, E., Istanti, R., Ardian, L. J., & Chotimah, S. C. (2019). Frailty State among Indonesian Elderly: Prevalence, Associated Factors, and Frailty State Transition. BMC Geriatrics, 19(1). https://doi.org/10.1186/S12877-019-1198-8
Soenarti, S., Mahendra, A. I., Rudijanto, A., Soeharto, S., Ratnawati, R., Maryunani, & Marintan, S. (2024). Cognitive Status and Low Sun Exposure as Frailty Major Risk Factor Among Older People in a Rural Area of East Java, Indonesia: A Cross-sectional Study. Geriatrics & Gerontology International, 24(S1), 170–175. https://doi.org/10.1111/GGI.14738
Vellas, B., Villars, H., Abellan, G., Soto, M. ., Rolland, Y., Guigoz, Y., Morley, J. ., Chumlea, W., Salva, A., Rubenstein, L. ., & Garry, P. (2006). Overview of The MNA® – Its History and Challenges. The Journal of Nutrition Health & Aging©, 10(6). https://www.researchgate.net/publication/6617786
WHO. (2020). Ageing and Health.
World Health Organization. (2020). Ageing.
Yu, Z., Kong, D., Peng, J., Wang, Z., & Chen, Y. (2021). Association of Malnutrition with All-cause Mortality in The Elderly Population: A 6-year Cohort Study. Nutrition, Metabolism, and Cardiovascular Diseases : NMCD, 31(1), 52–59. https://doi.org/10.1016/J.NUMECD.2020.08.004
Zhang, N., Jia, Z., Gu, T., Zheng, Y., Zhang, Y., Song, W., Chen, Z., Li, G., Tse, G., & Liu, T. (2023). Associations between modifiable risk factors and frailty: a Mendelian randomisation study. J Epidemiol Community Health, 77(12), 782–790. https://doi.org/10.1136/JECH-2023-220882
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Jurnal Ners dan Kebidanan (Journal of Ners and Midwifery)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.


 Student University of Muhammadiyah Malang - Indonesia
Student University of Muhammadiyah Malang - Indonesia
 Universitas Muhammadiyah Malang, Indonesia
Universitas Muhammadiyah Malang, Indonesia
 Sinta
Sinta ORCID
ORCID Scopus
Scopus
 Google Scholar
Google Scholar Scopus
Scopus Sinta
Sinta ORCID
ORCID







