The Moderating Role of Drinking Water Habit on the Effect of High- Purine Dietary Intake on Uric Acid Levels in Adults and the Elderly
DOI:
https://doi.org/10.26699/jnk.v12i3.ART.p259-269Keywords:
Drinking Water, High-Purine Diet, Hydration, Uric Acid, HyperuricemiaAbstract
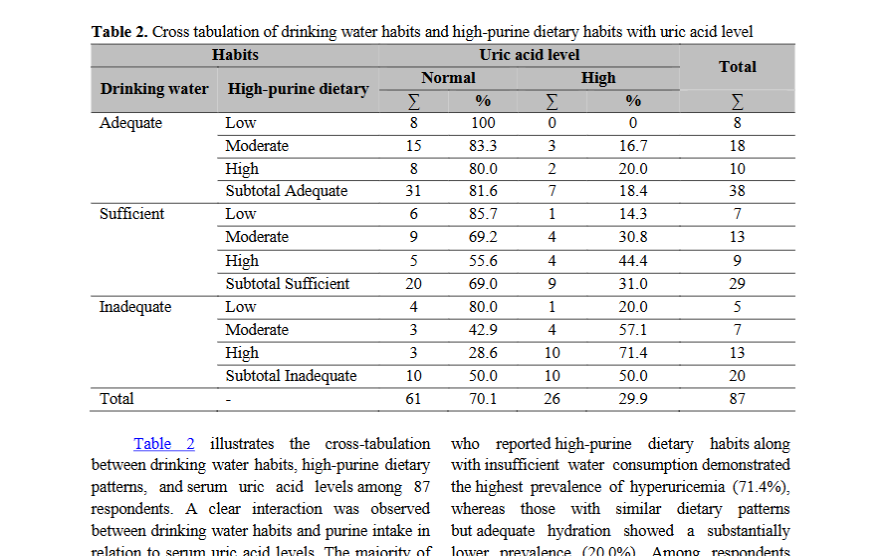
Serum uric acid levels are affected by dietary patterns and lifestyle factors. High-purine food consumption is a primary contributor to hyperuricemia, while hydration status may moderate this effect. This study aimed to examine the moderating role of drinking water habits on the relationship between high-purine dietary intake and serum uric acid levels among adults and the elderly. A cross-sectional design with purposive sampling was conducted, involving 87 respondents from Elderly Integrated Health Post (Posyandu Lansia). Data on purine-rich food intake and water-drinking habits were collected via structured questionnaires, and serum uric acid levels were measured using a point-of-care testing (POCT) device (Easy Touch GCU 3-in-1) with compatible test strips. Multiple logistic regression analysis assessed the interaction between purine intake and drinking water habits. Results revealed a significant association between high-purine dietary intake and elevated serum uric acid levels (p = 0.022). Participants who reported high-purine dietary habits along with insufficient water consumption demonstrated the highest prevalence of hyperuricemia (71.4%), whereas those with similar dietary patterns but adequate hydration showed a substantially lower prevalence (20.0%). A significant interaction effect (p = 0.040) indicated that sufficient water intake moderated the impact of a high-purine diet on uric acid levels. Adequate hydration thus plays a critical moderating role in reducing the adverse effects of a high-purine diet. Promoting sufficient water intake may serve as a simple and effective behavioral strategy to prevent hyperuricemia, particularly among individuals with high purine consumption.
References
Adomako, E. A., & Maalouf, N. M. (2023). Type 4 renal tubular acidosis and uric acid nephrolithiasis: two faces of the same coin? Current Opinion in Nephrology & Hypertension, 32(2), 145–152. https://doi.org/10.1097/MNH.0000000000000859
Aihemaitijiang, S., Zhang, Y., Zhang, L., Yang, J., Ye, C., Halimulati, M., Zhang, W., & Zhang, Z. (2020). The Association between Purine-Rich Food Intake and Hyperuricemia: A Cross-Sectional Study in Chinese Adult Residents. Nutrients, 12(12). https://doi.org/10.3390/nu12123835
Amin, Y., & Haswita, H. (2025). Identifying Purine Intake Among People with Gout and Its Relationship with Uric Acid Level: A Cross-Sectional Study. International Journal of Advanced Health Science and Technology, 5(3), 120–124. https://doi.org/10.35882/ijahst.v5i3.475
Anaizi, N. (2023). The impact of uric acid on human health: Beyond gout and kidney stones. Ibnosina Journal of Medicine and Biomedical Sciences, 15(03), 110–116. https://doi.org/10.1055/s-0043-1770929
Awwalina, I., Yunita Arini, S., Martiana, T., Ayuni Alayyannur, P., & Dwiyanti, E. (2022). RELATIONSHIP BETWEEN DRINKING WATER HABITS AND WORK CLIMATE PERCEPTIONS WITH DEHYDRATION INCIDENCE IN SHIPPING COMPANIES’WORKERS. The Indonesian Journal of Public Health, 17(1), 61–72. https://doi.org/10.20473/ijph.v17i1.2022.61-72
Bao, R., Chen, Q., Li, Z., Wang, D., Wu, Y., Liu, M., Zhang, Y., & Wang, T. (2022). Eurycomanol alleviates hyperuricemia by promoting uric acid excretion and reducing purine synthesis. Phytomedicine, 96, 153850. https://doi.org/10.1016/j.phymed.2021.153850
Beck, A. M., Seemer, J., Knudsen, A. W., & Munk, T. (2021). Narrative Review of Low-Intake Dehydration in Older Adults. In Nutrients (Vol. 13, Issue 9). https://doi.org/10.3390/nu13093142
Bruno, C., Collier, A., Holyday, M., & Lambert, K. (2021). Interventions to Improve Hydration in Older Adults: A Systematic Review and Meta-Analysis. Nutrients, 13(10). https://doi.org/10.3390/nu13103640
Calle Cárdenas, C. J., Morales Pilataxi, M. L., & Silva Ramos, M. V. (2024). Updated management of Gout. Interamerican Journal of Health Sciences, 4 SE-Review, 180. https://doi.org/10.59471/ijhsc2024.180
Chen, Z., Xue, X., Ma, L., Zhou, S., Li, K., Wang, C., Sun, W., Li, C., & Chen, Y. (2024). Effect of low-purine diet on the serum uric acid of gout patients in different clinical subtypes: a prospective cohort study. European Journal of Medical Research, 29(1), 449. https://doi.org/10.1186/s40001-024-02012-1
Chung, S., & Kim, G.-H. (2021). Urate Transporters in the Kidney: What Clinicians Need to Know. Electrolyte & Blood Pressure : E & BP, 19(1), 1–9. https://doi.org/10.5049/EBP.2021.19.1.1
Copur, S., Demiray, A., & Kanbay, M. (2022). Uric acid in metabolic syndrome: Does uric acid have a definitive role? European Journal of Internal Medicine, 103, 4–12. https://doi.org/10.1016/j.ejim.2022.04.022
Courbebaisse, M., Travers, S., Bouderlique, E., Michon-Colin, A., Daudon, M., De Mul, A., Poli, L., Baron, S., & Prot-Bertoye, C. (2023). Hydration for Adult Patients with Nephrolithiasis: Specificities and Current Recommendations. In Nutrients (Vol. 15, Issue 23). https://doi.org/10.3390/nu15234885
Čypienė, A., Gimžauskaitė, S., Rinkūnienė, E., Jasiūnas, E., Rugienė, R., Kazėnaitė, E., Ryliškytė, L., & Badarienė, J. (2023). The Association between Water Consumption and Hyperuricemia and Its Relation with Early Arterial Aging in Middle-Aged Lithuanian Metabolic Patients. In Nutrients (Vol. 15, Issue 3). https://doi.org/10.3390/nu15030723
Dalbeth, N., Gosling, A. L., Gaffo, A., & Abhishek, A. (2021). Gout. Lancet (London, England), 397(10287), 1843–1855. https://doi.org/10.1016/S0140-6736(21)00569-9
Danve, A., Sehra, S. T., & Neogi, T. (2021). Role of diet in hyperuricemia and gout. Best Practice & Research. Clinical Rheumatology, 35(4), 101723. https://doi.org/10.1016/j.berh.2021.101723
Dilokthornsakul, P., Louthrenoo, W., Chevaisrakul, P., Siripaitoon, B., Jatuworapruk, K., Upakdee, N., Buttham, B., & Towiwat, P. (2025). Impact of gout flare on health-related quality of life: a multi-center cross-sectional study in Thailand. Clinical Rheumatology, 44(3), 1317–1327. https://doi.org/10.1007/s10067-025-07339-6
Dório, M., Benseñor, I. M., Lotufo, P., Santos, I. S., & Fuller, R. (2022). Reference range of serum uric acid and prevalence of hyperuricemia: a cross-sectional study from baseline data of ELSA-Brasil cohort. Advances in Rheumatology, 62, 15. https://doi.org/10.1186/s42358-022-00246-3
Du, L., Zong, Y., Li, H., Wang, Q., Xie, L., Yang, B., Pang, Y., Zhang, C., Zhong, Z., & Gao, J. (2024). Hyperuricemia and its related diseases: mechanisms and advances in therapy. Signal Transduction and Targeted Therapy, 9(1), 212. https://doi.org/10.1038/s41392-024-01916-y
García-Nieto, V. M., Claverie-Martín, F., Moraleda-Mesa, T., Perdomo-Ramírez, A., Tejera-Carreño, P., Cordoba-Lanus, E., Luis-Yanes, M. I., & Ramos-Trujillo, E. (2022). Gout associated with reduced renal excretion of uric acid. Renal tubular disorder that nephrologists do not treat. Nefrología (English Edition), 42(3), 273–279. https://doi.org/10.1016/j.nefroe.2022.05.007
Gherghina, M.-E., Peride, I., Tiglis, M., Neagu, T. P., Niculae, A., & Checherita, I. A. (2022). Uric Acid and Oxidative Stress—Relationship with Cardiovascular, Metabolic, and Renal Impairment. In International Journal of Molecular Sciences (Vol. 23, Issue 6). https://doi.org/10.3390/ijms23063188
Jeong, H. G., & Park, H. (2022). Metabolic Disorders in Menopause. In Metabolites (Vol. 12, Issue 10). https://doi.org/10.3390/metabo12100954
Jing, Y., Ma, L., Zhang, Y., Li, X., Jiang, J., Long, J., & Ma, L. (2024). Impact of health literacy, social support, and socioeconomic position on the serum uric acid level in asymptomatic hyperuricaemia patients in China: a structural equation model. BMC Public Health, 24(1), 1606. https://doi.org/10.1186/s12889-024-19085-6
Kakutani-Hatayama, M., Kadoya, M., Okazaki, H., Kurajoh, M., Shoji, T., Koyama, H., Tsutsumi, Z., Moriwaki, Y., Namba, M., & Yamamoto, T. (2017). Nonpharmacological Management of Gout and Hyperuricemia: Hints for Better Lifestyle. American Journal of Lifestyle Medicine, 11(4), 321–329. https://doi.org/10.1177/1559827615601973
Kang, M., Baek, J. Y., Jo, Y., Ryu, D., Jang, I., Jung, H., & Kim, B. (2024). Higher serum uric acid as a risk factor for frailty in older adults: A nationwide population‐based study. Journal of Cachexia, Sarcopenia and Muscle, 15(5), 2134–2142. https://doi.org/10.1002/jcsm.13561
Kang, S., Kwon, D., Lee, J., Chung, Y.-J., Kim, M.-R., Namkung, J., & Jeung, I. C. (2021). Association between Serum Uric Acid Levels and Bone Mineral Density in Postmenopausal Women: A Cross-Sectional and Longitudinal Study. In Healthcare (Vol. 9, Issue 12). https://doi.org/10.3390/healthcare9121681
Kim, H. J. (2024). Association Between Hyperuricemia and Dehydration in Children With Acute Gastroenteritis. Pediatric Emergency Care, 10–1097. https://doi.org/10.1097/PEC.0000000000003498
Kuwabara, M., Hisatome, I., Ae, R., Kosami, K., Aoki, Y., Andres-Hernando, A., Kanbay, M., & Lanaspa, M. A. (2025). Hyperuricemia, A new cardiovascular risk. Nutrition, Metabolism and Cardiovascular Diseases, 35(3), 103796. https://doi.org/https://doi.org/10.1016/j.numecd.2024.103796
Liu, P., Kadier, K., Wu, X., Xiangyu, S., Zhang, G., Liu, X., Song, D., & Cui, C. (2025). Association between higher estimated glucose disposal rate and reduced prevalence of hyperuricemia and gout. Frontiers in Nutrition, 12, 1658286. https://doi.org/10.3389/fnut.2025.1658286
Maharani, T. D., Ayuningtyas, K. K., Nurhani, A. S., Sitasari, A., Wijanarka, A., & Siswati, T. (2025). Relation between high purine intake and hiperurisemia in pre-elderly to late elderly ages. Nutrition and Health Insights, 2(1), 34–38. https://doi.org/10.63197/nahi.v2i1.24
Nishizawa, H., Maeda, N., & Shimomura, I. (2022). Impact of hyperuricemia on chronic kidney disease and atherosclerotic cardiovascular disease. Hypertension Research, 45(4), 635–640. https://doi.org/10.1038/s41440-021-00840-w
Otani, N., Ouchi, M., Misawa, K., Hisatome, I., & Anzai, N. (2022). Hypouricemia and Urate Transporters. In Biomedicines (Vol. 10, Issue 3). https://doi.org/10.3390/biomedicines10030652
Pence, J., Davis, A., Allen-Gregory, E., & Bloomer, R. J. (2025). Hydration Strategies in Older Adults. In Nutrients (Vol. 17, Issue 14). https://doi.org/10.3390/nu17142256
Stookey, J. D., & Kavouras, S. A. (2020). Water Researchers Do Not Have a Strategic Plan for Gathering Evidence to Inform Water Intake Recommendations to Prevent Chronic Disease. In Nutrients (Vol. 12, Issue 11). https://doi.org/10.3390/nu12113359
Wang, H., Xie, L., Song, X., Wang, J., Li, X., Lin, Z., Su, T., Liang, B., & Huang, D. (2022). Purine-induced IFN-γ promotes uric acid production by upregulating xanthine oxidoreductase expression. Frontiers in Immunology, 13, 773001. https://doi.org/10.3389/fimmu.2022.773001
Wen, Z.-Y., Wei, Y.-F., Sun, Y.-H., & Ji, W.-P. (2024). Dietary pattern and risk of hyperuricemia: an updated systematic review and meta-analysis of observational studies. Frontiers in Nutrition, Volume 11-2024. https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1218912
Winder, M., Owczarek, A. J., Mossakowska, M., Broczek, K., Grodzicki, T., Wierucki, Ł., & Chudek, J. (2021). Prevalence of Hyperuricemia and the Use of Allopurinol in Older Poles—Results from a Population-Based PolSenior Study. In International Journal of Environmental Research and Public Health (Vol. 18, Issue 2). https://doi.org/10.3390/ijerph18020387
Xiang, D., Yuan, L., Wu, Y., Yuan, Y., Liao, S., Chen, W., Zhang, M., Zhang, Q., Ding, L., & Wang, Y. (2025). Knowledge, Attitude, and Practice Toward Hyperuricemia Among Patients Diagnosed with Hyperuricemia. Journal of Multidisciplinary Healthcare, 18(null), 2845–2858. https://doi.org/10.2147/JMDH.S512887
Zhang, Y., Chen, S., Yuan, M., Xu, Y., & Xu, H. (2022). Gout and Diet: A Comprehensive Review of Mechanisms and Management. In Nutrients (Vol. 14, Issue 17). https://doi.org/10.3390/nu14173525
Zhao, M., Jian, J., Yang, D., Sun, H., Liu, L., Yan, Z., Ma, Y., & Zhao, Y. (2024). Knowledge, attitudes, and practices of gouty arthritis in the general population aged > 30. BMC Medical Education, 24(1), 775. https://doi.org/10.1186/s12909-024-05690-x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Jurnal Ners dan Kebidanan (Journal of Ners and Midwifery)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.


 STIKes Patria Husada Blitar, Indonesia
STIKes Patria Husada Blitar, Indonesia Google Scholar
Google Scholar Sinta
Sinta ORCID
ORCID
 STIKes Patria Husada Blitar, Indonesia
STIKes Patria Husada Blitar, Indonesia Google Scholar
Google Scholar Sinta
Sinta ORCID
ORCID



