Medication and Lifestyle Modification Adherence to Blood Pressure Control Among Hypertensive Patients: A Cross-Sectional Study
DOI:
https://doi.org/10.26699/jnk.v12i3.ART.p221-229Keywords:
Adherence to Medication, Lifestyle Modification, Blood PressureAbstract
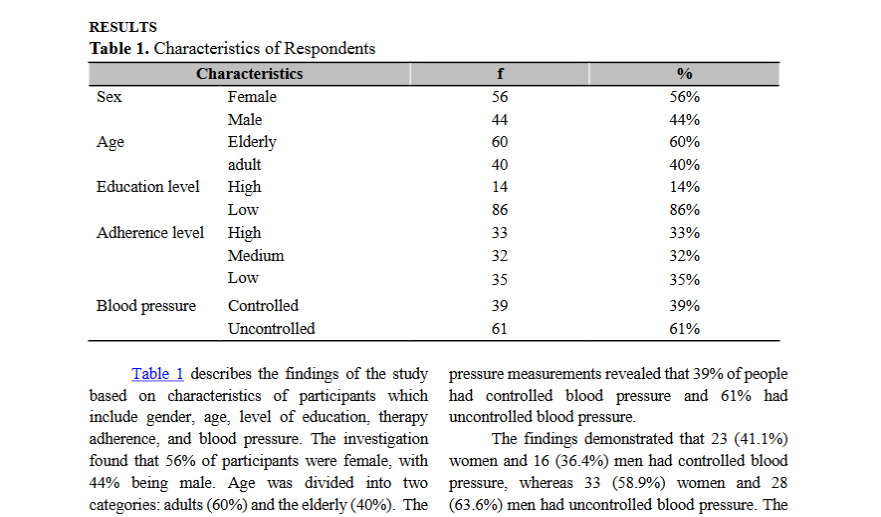
Adherence to medication is a crucial aspect in blood pressure control, which in turn leads to a reduction in the incidence of cardiovascular disease and medical costs. The aim of the study was to determine medication and lifestyle modifications adherence to blood pressure control among hypertensive patients in a public health center. The method of the study used a cross-sectional involving participants with primary hypertension at the Community Health Centre. One hundred respondents were recruited through consecutive sampling methods. Hypertensive patients aged 40 to 74 years who has been taking antihypertensive drugs for at least two months were approved, while hypertensive patients with cormobid and patients with communicative or behavioral impairments were excluded. The instruments used was the TAQPH, which consists of six factors: medication, diet, stimulus, weight control, physical exercise, and stress management. Blood pressure measurements were conducted using a mercury sphygmomanometer. The data was examined with the chi-squared statistical test. Twenty-five (75%) of the patients who demonstrated high levels of adherence had controlled blood pressure. In contrast, 24 (75.0%) patients with medium adherence and 29 (82.9%) patients with low adherence demonstrated uncontrolled blood pressure. A significant correlation was observed between the level of therapy adherence and blood pressure in hypertensive patients (p = 0.001). Patients with low to moderate levels of adherence have uncontrolled blood pressure, whereas those with high levels of adherence have controlled blood pressure.
References
Adisa, R., Ilesanmi, O. A., & Fakeye, T. O. (2018). Treatment adherence and blood pressure outcome among hypertensive out-patients in two tertiary hospitals in Sokoto, Northwestern Nigeria. BMC Cardiovascular Disorders, 18(1), 1–10. https://doi.org/10.1186/s12872-018-0934-x
Alhawassi, T. M., Krass, I., & Pont, L. G. (2015). Hypertension in Older Persons: A Systematic Review of National and International Treatment Guidelines. Journal of Clinical Hypertension, 17(6), 486–492. https://doi.org/10.1111/jch.12536
Amaral, O., Chaves, C., Duarte, J., Coutinho, E., Nelas, P., & Preto, O. (2015). Treatment Adherence in Hypertensive Patients – A Cross-sectional Study. Procedia - Social and Behavioral Sciences, 171, 1288–1295. https://doi.org/10.1016/j.sbspro.2015.01.243
Asgedom, S. W., Atey, T. M., & Desse, T. A. (2018). Antihypertensive medication adherence and associated factors among adult hypertensive patients at Jimma University Specialized Hospital, southwest Ethiopia. BMC Research Notes, 11(1), 1–8. https://doi.org/10.1186/s13104-018-3139-6
Butler, M. J., Tanner, R. M., Muntner, P., Shimbo, D., Bress, A. P., Shallcross, A. J., Sims, M., Ogedegbe, G., & Spruill, T. M. (2017). Adherence to antihypertensive medications and associations with blood pressure among African Americans with hypertension in the Jackson Heart Study. Journal of the American Society of Hypertension, 11(9), 581-588.e5. https://doi.org/10.1016/j.jash.2017.06.011
Chowdhury, M. A. B., Uddin, M. J., Haque, M. R., & Ibrahimou, B. (2016). Hypertension among adults in Bangladesh: Evidence from a national cross-sectional survey. BMC Cardiovascular Disorders, 16(1), 1–10. https://doi.org/10.1186/s12872-016-0197-3
Depkes RI. (2018). Laporan Riskesdas 2018 Nasional.pdf. In Lembaga Penerbit Balitbangkes (p. 156).
Edward, A., Campbell, B., Manase, F., & Appel, L. J. (2021). Patient and healthcare provider perspectives on adherence with antihypertensive medications: an exploratory qualitative study in Tanzania. BMC Health Services Research, 21(1), 1–12. https://doi.org/10.1186/s12913-021-06858-7
Erin C. Dowd, Michael J. Frank, Anne Collins, James M. Goldd, and Deanna M. Barch, & Kuschner. (2017). SPRINT: Intensive vs SBP COntrol and CVD Outcomes in Adults Aged 75+. Physiology & Behavior, 176(3), 139–148. https://doi.org/10.1001/jama.2016.7050.Intensive
Esquivel Garzón, N., & Díaz Heredia, L. P. (2019). Validity and Reliability of the Treatment Adherence Questionnaire for Patients with Hypertension. Investigacion y Educacion En Enfermeria, 37(3). https://doi.org/10.17533/udea.iee.v37n3e09
Kang, C. D., Tsang, P. P. M., Li, W. T. L., Wang, H. H. X., Liu, K. Q. L., Griffiths, S. M., & Wong, M. C. S. (2015). Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: A cross-sectional study. International Journal of Cardiology, 182(C), 250–257. https://doi.org/10.1016/j.ijcard.2014.12.064
Kapoor, M., Dhar, M., Mirza, A., Saxena, V., & Pathania, M. (2021). Factors responsible for Uncontrolled Hypertension in the Adults over 50 years of age : A pilot study from Northern India. Indian Heart Journal, 73(5), 644–646. https://doi.org/10.1016/j.ihj.2021.07.003
Liberty, I. A., Pariyana, P., Roflin, E., & Waris, L. (2018). Determinan Kepatuhan Berobat Pasien Hipertensi Pada Fasilitas Kesehatan Tingkat I. Jurnal Penelitian Dan Pengembangan Pelayanan Kesehatan, 1(1), 58–65. https://doi.org/10.22435/jpppk.v1i1.428
Macquart de Terline, D., Kramoh, K. E., Bara Diop, I., Nhavoto, C., Balde, D. M., Ferreira, B., Houenassi, M. D., Hounsou, D., Ikama, M. S., Kane, A., Kimbally-Kaki, S. G., Kingue, S., Koffi, F., Kouam Kouam, C., Limbole, E., Mfeukeu Kuate, L., Mipinda, J. B., N’goran, Y., Sesso, Z., … Antignac, M. (2020). Poor adherence to medication and salt restriction as a barrier to reaching blood pressure control in patients with hypertension: Cross-sectional study from 12 sub-Saharan countries. Archives of Cardiovascular Diseases, 113(6–7), 433–442. https://doi.org/10.1016/j.acvd.2019.11.009
Mitra, M., & Wulandari, W. (2019). Factors affecting uncontrolled blood pressure among elderly hypertensive patients in Pekanbaru City, Indonesia. Open Access Macedonian Journal of Medical Sciences, 7(7), 1209–1213. https://doi.org/10.3889/oamjms.2019.255
Omboni, S., & Ferrari, R. (2015). The Role of Telemedicine in Hypertension Management: Focus on Blood Pressure Telemonitoring. Current Hypertension Reports, 17(4), 1–13. https://doi.org/10.1007/s11906-015-0535-3
Pan, J., Wu, L., Wang, H., Lei, T., Hu, B., Xue, X., & Li, Q. (2019). Determinants of hypertension treatment adherence among a Chinese population using the therapeutic adherence scale for hypertensive patients. Medicine (United States), 98(27), e16116. https://doi.org/10.1097/MD.0000000000016116
Peacock, E., & Krousel-Wood, M. (2017). Adherence to Antihypertensive Therapy. Medical Clinics of North America, 101(1), 229–245. https://doi.org/10.1016/j.mcna.2016.08.005
Piña, I. L., Di Palo, K. E., Brown, M. T., Choudhry, N. K., Cvengros, J., Whalen, D., Whitsel, L. P., & Johnson, J. (2020). Medication adherence: Importance, issues and policy: A policy statement from the American Heart Association. Progress in Cardiovascular Diseases. https://doi.org/10.1016/j.pcad.2020.08.003
Pramana, galih adi, Setia, R., & Saputri, D. N. E. (2019). Faktor-faktor yang Mempengaruhi Kepatuhan Minum Obat Pasien Hipertensi Peserta Prolanis di Puskesmas Pringapus Kabupaten Semarang. Indonesian Journal of Pharmacy and Natural Product, 02(01), 19–24. https://doi.org/10.35473/ijpnp.v2i1.196
Qodir, A. (2020). Analisis Faktor Determinan yang berhubungan dengan Kepatuhan Rekomendasi Modifikasi Gaya Hidup Pasien Hipertensi. Jurnal Ners Dan Kebidanan (Journal of Ners and Midwifery), 7(2), 256–263. https://doi.org/10.26699/jnk.v7i2.art.p256-263
Rahman, M., Williams, G., & Al Mamun, A. (2017). Gender differences in hypertension awareness, antihypertensive use and blood pressure control in Bangladeshi adults: findings from a national cross-sectional survey. Journal of Health, Population, and Nutrition, 36(1), 23. https://doi.org/10.1186/s41043-017-0101-5
Shankari, G., Ng, S. C., Goh, S. Y., Woon, F. P., Doshi, K., Wong, P. S., Fan, Q., Tan, I. F., Narasimhalu, K., & De Silva, D. A. (2020). Modifiable Factors Associated with Non-Adherence to Secondary Ischaemic Stroke Prevention Strategies. Journal of Stroke and Cerebrovascular Diseases, 29(12), 105395. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105395
Taylor, M. K., Sullivan, D. K., Ellerbeck, E. F., Gajewski, B. J., & Gibbs, H. D. (2019). Nutrition literacy predicts adherence to healthy/unhealthy diet patterns in adults with a nutrition-related chronic condition. Public Health Nutrition, 22(12), 2157–2169. https://doi.org/10.1017/S1368980019001289
Teshome, D. F., Bekele, K. B., Habitu, Y. A., & Gelagay, A. A. (2017). Medication adherence and its associated factors among hypertensive patients attending the Debre Tabor General Hospital, Northwest Ethiopia. Integrated Blood Pressure Control, 10, 1–7. https://doi.org/10.2147/IBPC.S128914
Tibebu, A., & Mengistu, D. (2017). Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa , Ethiopia. 323–330. https://doi.org/10.2147/PPA.S126382
Vrijens, B., Antoniou, S., Burnier, M., & Sierra, A. De. (2017). Current Situation of Medication Adherence in Hypertension. 8(March), 1–8. https://doi.org/10.3389/fphar.2017.00100
Yang, Q., Chang, A., Ritchey, M. D., & Loustalot, F. (2017). Antihypertensive Medication Adherence and Risk of Cardiovascular Disease Among Older Adults: A Population-Based Cohort Study. Journal of the American Heart Association, 6(6). https://doi.org/10.1161/JAHA.117.006056
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Jurnal Ners dan Kebidanan (Journal of Ners and Midwifery)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.


 STIKes Widyagama Husada Malang, Indonesia
STIKes Widyagama Husada Malang, Indonesia Google Scholar
Google Scholar Sinta
Sinta
 STIKes Widyagana Husada Malang, Indonesia
STIKes Widyagana Husada Malang, Indonesia Google Scholar
Google Scholar Scopus
Scopus Sinta
Sinta ORCID
ORCID




