Improving Knowledge about Drug Use During Fasting through Pharmaceutical Counseling Accompanied by Leaflet
DOI:
https://doi.org/10.26699/jcsh.v6i1.1196Keywords:
Pharmaceutical Counseling, Leaflet, FastingAbstract
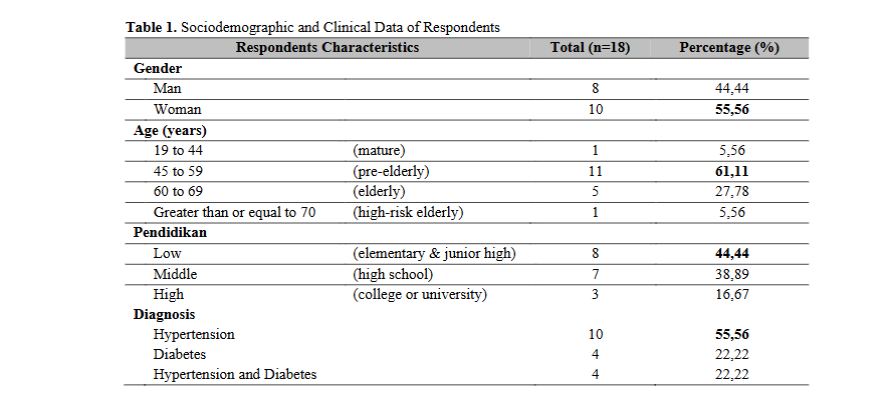
Medication use in patients with chronic diseases during Ramadan is a crucial yet often overlooked public health challenge in the primary health care system in Indonesia. Non-compliance with medication regimens and inappropriate dosage adjustments during fasting can lead to serious complications and even medical emergencies, especially in patients with diabetes and hypertension. This community service activity aimed to evaluate the effectiveness of pharmaceutical counseling, accompanied by leaflets, in enhancing patients’ knowledge of medication use during fasting for chronic conditions. This quasi-experimental study was conducted at the Technical Implementing Unit of Kepanjenkidul Health Center, Blitar City, involving 18 patients diagnosed with diabetes and hypertension. The study employed a knowledge questionnaire. The design of this study aims to analyze changes in patient knowledge related to drug use during Ramadan fasting through a structured intervention approach. The results of the activity showed a significant increase in knowledge scores, from an average of 28.33 (pre-test) to 47.11 (post-test), representing a percentage increase of 37.56% (p-value = 0.000, p = < 0.05). In conclusion, pharmaceutical counseling through brochures has shown promise as a strategy for improving patients’ understanding of medication management during Ramadan. It is recommended that health centers develop specific counseling protocols and educational materials tailored to the characteristics of patients, particularly those from low-educated and pre-elderly groups. The implementation of this counseling program needs to be integrated into routine pharmaceutical services, with a focus on preparation several weeks before Ramadan to improve medication safety and therapy fulfillment for patients who choose to fast.
References
Abu, H., Aboumatar, H., Carson, K. A., Goldberg, R., Cooper, L. A., & Bloomberg, J. H. (2020). HHS Public Access. Eur J Pers Cent Healthc, 6(1), 108–114. https://doi.org/10.5750/ejpch.v6i1.1416.Hypertension
Aghazadeh, S., & Aldoory, L. (2023). Public Relations Theory III (1st Edition). Taylor & Francis Online. https://doi.org/10.4324/9781003141396-27
Al Rifai, L. A., Soubra, L., Hassanein, M., & Amin, M. E. K. (2022). Comprehensive care for patients with diabetes in Ramadan: A module for pharmacy students and pharmacists. Saudi Pharmaceutical Journal, 30(5), 619–628. https://doi.org/10.1016/J.JSPS.2022.02.008
Almansour, H. A., Chaar, B., & Saini, B. (2017). Pharmacists’ perspectives about their role in care of patients with diabetes observing Ramadan. Research in Social and Administrative Pharmacy, 13(1), 109–122. https://doi.org/10.1016/J.SAPHARM.2016.02.006
Amin, M. E. K., Qudah, B. A., Kaur, A., Rawy, M., & Chewning, B. (2021). Construction and evaluation of an online module addressing counseling patients with diabetes observing religious fasting. Currents in Pharmacy Teaching and Learning, 13(12), 1602–1610. https://doi.org/10.1016/J.CPTL.2021.09.022
Babb, S. J. (2022). Meeting the Needs of Nontraditional Undergraduate Students. https://doi.org/DOI: 10.4018/978-1-7998-8323-4.ch004
Bates, J., Schrewe, B., & Ellaway, R. H. (2018). medical education in review Embracing standardisation and contextualisation in medical education. Medical Education, 1–10. https://doi.org/10.1111/medu.13740
Bouchareb, S., Chrifou, R., Bourik, Z., & Nijpels, G. (2022). “ I am my own doctor ”: A qualitative study of the perspectives and decision-making process of Muslims with diabetes on Ramadan fasting. 1, 1–18. https://doi.org/10.1371/journal.pone.0263088
Chaudhary, G., Navyashree, M., Roy, D. Sen, & Srinivasan, R. (2017). A Study On Effect Of Pharmacist Mediated Patient Counseling In Hypertensive Patients In Terms Of Knowledge , Compliance And Quality Of Life . Journal of Pharmacy and Biological Sciences, 12(3), 46–54. https://doi.org/10.9790/3008-1203024654
Creswell. JW, C. J. (2018). Research Design. In M. O’Heffernan (Ed.), Writing Center Talk over Time (Fifth Edit). SAGE Publications. https://doi.org/10.4324/9780429469237-3
Fatiha, C. N., & Firdaus, M. (2023). Education on drug use during Ramadan. Community Empowerment, 8(1), 56–62. https://doi.org/10.31603/ce.8066
Grindrod, K., & Alsabbagh, W. (2017). Managing medications during Ramadan fasting. Canadian Pharmacists Journal, 150(3), 146–149. https://doi.org/10.1177/1715163517700840
Habas, E., Errayes, M., Habas, E., Farfar, K. L., Alfitori, G., Habas, A. E., Rayani, A., & Elzouki, A.-N. Y. (2022). Fasting Ramadan in Chronic Kidney Disease (CKD), Kidney Transplant and Dialysis Patients: Review and Update. Cureus, 14(5), e25269. https://doi.org/10.7759/cureus.25269
Hassanein, M., Afandi, B., Yakoob Ahmedani, M., Mohammad Alamoudi, R., Alawadi, F., Bajaj, H. S., Basit, A., Bennakhi, A., El Sayed, A. A., Hamdy, O., Hanif, W., Jabbar, A., Kleinebreil, L., Lessan, N., Shaltout, I., Mohamad Wan Bebakar, W., Abdelgadir, E., Abdo, S., Al Ozairi, E., … Binte Zainudin, S. (2022). Diabetes and Ramadan: Practical guidelines 2021. Diabetes Research and Clinical Practice, 185(January), 109185. https://doi.org/10.1016/j.diabres.2021.109185
Hening, W., Sartika, R. D., & Sauriasari, R. (2019). Effect of hospital pharmacist counseling on clinical outcomes of type 2 diabetes mellitus outpatients. Journal of Research in Pharmacy Practice, 8(3), 155. https://doi.org/10.4103/jrpp.jrpp_19_67
Holst, C., Stelzle, D., Diep, L. M., & Sukums, F. (2022). Improving Health Knowledge Through Provision of Free Digital Health Education to Rural Communities in Iringa , Tanzania : Nonrandomized Intervention Study Corresponding Author : Journal of Medical Internet Research, 24, 1–14. https://doi.org/10.2196/37666
Kavit, M. A. A. A., Purnami, C. T., Agushybana, F., & Dharminto, D. (2022). Hubungan Faktor Demografi dengan Literasi Kesehatan tentang Penyakit tidak Menular pada Lansia. Jurnal Manajemen Kesehatan Indonesia, 10(2), 95–105. https://doi.org/10.14710/jmki.10.2.2022.95-105
Lambert, S., Lynn, J., Ould, L., Belzile, E., Maria, A., Folch, N., Rosenberg, E., Maheu, C., Ciofani, L., Dubois, S., Gélinas-phaneuf, E., Drouin, S., Leung, K., Tremblay, S., Clayberg, K., & Ciampi, A. (2021). Patient Education and Counseling The effect of culturally-adapted health education interventions among culturally and linguistically diverse ( CALD ) patients with a chronic illness : A meta-analysis and descriptive systematic review. Patient Education and Counseling, 104(7), 1608–1635. https://doi.org/10.1016/j.pec.2021.01.023
Lazzeroni, D. (2020). Health literacy in cardiovascular prevention: ‘From small things, big things come.’ European Journal of Preventive Cardiology, 27(2), 206–208. https://doi.org/10.1177/2047487319888812
Lu, J., Sun, S., Gu, Y., Li, H., Fang, L., Zhu, X., & Xu, H. (2023). Health literacy and health outcomes among older patients suffering from chronic diseases: A moderated mediation model. Front Public Health, 10(10), 1069174. https://doi.org/10.3389/fpubh.2022.1069174
Ozturk, G. Z., Egici, M. T., Sagsoz, O., & Bukhari, M. H. (2021). Evaluating the effect of Ramadan Fasting on patients with chronic diseases. Pakistan Journal of Medical Sciences, 37(4), 1–6. https://doi.org/10.12669/pjms.37.4.3199
Patel, N. R., Kennedy, A., Blickem, C., Rogers, A., Reeves, D., & Chew-Graham, C. (2015). Having diabetes and having to fast: A qualitative study of British Muslims with diabetes. Health Expectations, 18(5), 1698–1708. https://doi.org/10.1111/hex.12163
Pintz, C., Posey, L., Farmer, P., & Pearl, Q. (2021). Nurse Education in Practice Interprofessional care of people with multiple chronic conditions : An open-access resource for nursing educators. Nurse Education in Practice, 51(February), 102990. https://doi.org/10.1016/j.nepr.2021.102990
Rampamba, E. M., Meyer, J. C., A, H. E., & Godman, B. (2019). Empowering Hypertensive Patients in South Africa to Improve Their Disease Management: A Pharmacist-Led Intervention. J Res Pharm Pract, 8(4), 208–213. https://doi.org/10.4103/jrpp.JRPP_18_74
Schmitz, J., Kamping, S., Wiegratz, J., Maike, M., Stork, J., Colloca, L., Flor, H., & Klinger, R. (2017). Impact of patient information leaflets on pain medication intake behavior : a pilot study. 2, 1–6.
Shiju, R., Akhil, A., Thankachan, S., Tuomilehto, J., Arouj, M. A., & Bennakhi, A. (2022). Safety Assessment of Glucose-Lowering Drugs and Importance of Structured Education during Ramadan: A Systematic Review and Meta-Analysis. Journal of Diabetes Research, 2022(1), 3846253. https://doi.org/10.1155/2022/3846253
Sustersic, M., Tissot, M., Tyrant, J., Gauchet, A., Foote, A., Vermorel, C., & Bosson, J. L. (2019). Impact of patient information leaflets on doctor-patient communication in the context of acute conditions: a prospective, controlled, before-after study in two French emergency departments. BMJ Open, 9, 24184. https://doi.org/10.1136/bmjopen-2018-024184
Tourkmani, A. M., Azmi Hassali, M., Alharbi, T. J., Alkhashan, H. I., Alobikan, A. H., Bakhiet, A. H., Alqahtani, H. B., Alrasheedy, A. A., Alawwad, A. D., Mishriky, A. M., & Aljadhey, H. (2016). Impact of ramadan focused education program on hypoglycemic risk and metabolic control for patients with type 2 diabetes. Patient Preference and Adherence, 10, 1709–1717. https://doi.org/10.2147/PPA.S113324


 Universitas STRADA Indonesia Kediri, Indonesia
Universitas STRADA Indonesia Kediri, Indonesia Google Scholar
Google Scholar Sinta
Sinta ORCID
ORCID Scopus
Scopus




