Enhancing Clinical Competence of New Graduate Nurses to Improve The Quality of Patient Care
DOI:
https://doi.org/10.26699/jnk.v12i1.ART.p051-063Keywords:
Clinical Competence, Enhancement, New Graduate Nurses, Public Hospitals, Quality Patient CareAbstract
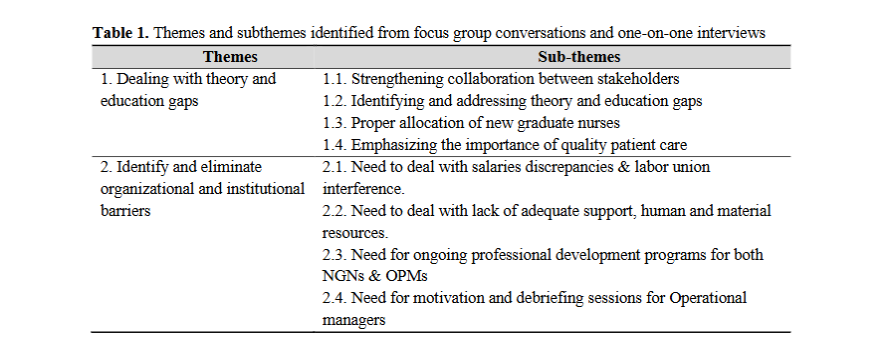
Nurses are expected to be competent with the ability to perform independently and deliver safe patient care. This paper aimed to report the measures to enhance the clinical competence of new graduate nurses with the intention of improving quality of patient care in public hospitals. This research was a qualitative design with focus group discussions and individual interviews used to collect data from seven public hospitals in three districts of Northwest Province, South Africa, during the period, of September, and November 2021. Thematic data analysis was employed to analyze the collected data. The result of this research was two themes with eight sub-themes reported as follows: 1) Dealing with theory and education gaps, and 2) Identify and eliminate organizational and institutional barriers. The conclusion was a theory-practice gap can lead to a lack of confidence and incompetence which will in return hinder safe practice and quality performance. On the other hand, organizational and institutional challenges can compromise support for newly graduated nurses during their transition period. Therefore, attending to the measures to enhance new graduate nurses’ clinical competence will benefit the healthcare facilities, as it would have positive effects on patient care. It is therefore suggested that future studies may use different study methods including the different populations such as the new graduate nurses themselves, and operational managers from the other healthcare facilities such as clinics and primary healthcare centers.
References
Africa, L., & Shinners, J. S. (2020). Tracking medical errors and near misses in the new graduate registered nurse. Nursing Forum, 55(2), 174–176. https://doi.org/10.1111/nuf.12412
Amsalu, B., Fekadu, T., Mengesha, A., & Bayana, E. (2020). Clinical practice competence of mettu university nursing students: A cross-sectional study. Advances in Medical Education and Practice, 11, 791–798. https://doi.org/10.2147/AMEP.S267398
Baljoon, R., Banjar, H., & Banakhar, M. (2018). Nurses’ Work Motivation and the Factors Affecting It: A Scoping Review. International Journal of Nursing & Clinical Practices, 5(1). https://doi.org/10.15344/2394-4978/2018/277
Boamah, S. A., Read, E. A., & Spence Laschinger, H. K. (2017). Factors influencing new graduate nurse burnout development, job satisfaction and patient care quality: a time-lagged study. Journal of Advanced Nursing, 73(5), 1182–1195. https://doi.org/10.1111/jan.13215
Brenner, M. J., Pandian, V., Milliren, C. E., Graham, D. A., Zaga, C., Morris, L. L., Bedwell, J. R., Das, P., Zhu, H., Lee Y. Allen, J., Peltz, A., Chin, K., Schiff, B. A., Randall, D. M., Swords, C., French, D., Ward, E., Sweeney, J. M., Warrillow, S. J., … Roberson, D. W. (2020). Global Tracheostomy Collaborative: data-driven improvements in patient safety through multidisciplinary teamwork, standardisation, education, and patient partnership. In British Journal of Anaesthesia (Vol. 125, Issue 1, pp. e104–e118). Elsevier Ltd. https://doi.org/10.1016/j.bja.2020.04.054
Chen, Q., Lan, X., Zhao, Z., Hu, S., Tan, F., Gui, P., & Yao, S. (2020). Role of Anesthesia Nurses in the Treatment and Management of Patients With COVID-19. Journal of Perianesthesia Nursing, 35(5), 453–456. https://doi.org/10.1016/j.jopan.2020.05.007
Creswell, J. W., & Creswell, J. D. (2018). Research Design: Qualitative, Quantitative, and Mixed Methods Approaches: Vol. Fifth Edition. SAGE Publication.
Dilles, T., Heczkova, J., Tziaferi, S., Helgesen, A. K., Grøndahl, V. A., Van Rompaey, B., Sino, C. G., & Jordan, S. (2021). Nurses and pharmaceutical care: Interprofessional, evidence-based working to improve patient care and outcomes. In International Journal of Environmental Research and Public Health (Vol. 18, Issue 11). MDPI AG. https://doi.org/10.3390/ijerph18115973
Faraji, A., Karimi, M., Azizi, S. M., Janatolmakan, M., & Khatony, A. (2019). Evaluation of clinical competence and its related factors among ICU nurses in Kermanshah-Iran: A cross-sectional study. International Journal of Nursing Sciences, 6(4), 421–425. https://doi.org/10.1016/j.ijnss.2019.09.007
Gautam, S., Poudel, A., Paudyal, K., & Prajapati, M. M. (2023). Transition to professional practice: Perspectives of new nursing graduates of Nepal. BMC Nursing, 22(1). https://doi.org/10.1186/s12912-023-01418-2
Goldsberry, J. W. (2018). Advanced practice nurses leading the way: Interprofessional collaboration. In Nurse Education Today (Vol. 65, pp. 1–3). Churchill Livingstone. https://doi.org/10.1016/j.nedt.2018.02.024
Gray, J. R., Grove, S. K. G., & Sutherland, S. (2016). Burns and Grove’s The Practice of Nursing Research - E-Book: Appraisal, synthesis, and generation of evidence. Elsevier Health Sciences.
Guillaume, & Kirton. (n.d.). Unions defending and promoting nursing and midwifery: workplace challenges, activity and strategies. https://www.researchgate.net/publication/344403962
Huang, L. H., Chen, C. M., Chen, S. F., & Wang, H. H. (2020). Roles of nurses and National Nurses Associations in combating COVID-19: Taiwan experience. International Nursing Review, 67(3), 318–322. https://doi.org/10.1111/inr.12609
ICN. (2023). Position Statement: Patient Safety [Internet]. www.icn.ch
Jarva, E., Oikarinen, A., Andersson, J., Tuomikoski, A. M., Kääriäinen, M., Meriläinen, M., & Mikkonen, K. (2022). Healthcare professionals’ perceptions of digital health competence: A qualitative descriptive study. Nursing Open, 9(2), 1379–1393. https://doi.org/10.1002/nop2.1184
Kiernan, & Olsen. (2020). Improving clinical competency using simulation technology. Learning Curve, 50(7). www.Nursing2020.com
Kuokkanen, L., Leino-Kilpi, H., Numminen, O., Isoaho, H., Flinkman, M., & Meretoja, R. (2016). Newly graduated nurses’ empowerment regarding professional competence and other work-related factors. BMC Nursing, 15(1). https://doi.org/10.1186/s12912-016-0143-9
Labrague, L. J., Al Sabei, S., Al Rawajfah, O., AbuAlRub, R., & Burney, I. (2022). Interprofessional collaboration as a mediator in the relationship between nurse work environment, patient safety outcomes and job satisfaction among nurses. Journal of Nursing Management, 30(1), 268–278. https://doi.org/10.1111/jonm.13491
Lee, S. E., & Dahinten, V. S. (2020). The Enabling, Enacting, and Elaborating Factors of Safety Culture Associated With Patient Safety: A Multilevel Analysis. Journal of Nursing Scholarship, 52(5), 544–552. https://doi.org/10.1111/jnu.12585
Lindfors, K., Flinkman, M., Kaunonen, M., Huhtala, H., & Paavilainen, E. (2022). New graduate registered nurses’ professional competence and the impact of preceptors’ education intervention: a quasi-experimental longitudinal intervention study. BMC Nursing, 21(1). https://doi.org/10.1186/s12912-022-01133-4
Matlhaba, K. L. (2022). Compulsory Community Service for New Nurse Graduates in South Africa: A Narrative Literature Review. In 66 Journal of Nursing Regulation. www.journalofnursingregulation.com
Moloney, W., Fieldes, J., & Jacobs, S. (2020). An integrative review of how healthcare organizations can support hospital nurses to thrive at work. In International Journal of Environmental Research and Public Health (Vol. 17, Issue 23, pp. 1–21). MDPI. https://doi.org/10.3390/ijerph17238757
Müller, J., & Couper, I. (2021). Preparing Graduates for Interprofessional Practice in South Africa: The Dissonance Between Learning and Practice. Frontiers in Public Health, 9. https://doi.org/10.3389/fpubh.2021.594894
Naeem, M., Ozuem, W., Howell, K., & Ranfagni, S. (2023). A Step-by-Step Process of Thematic Analysis to Develop a Conceptual Model in Qualitative Research. International Journal of Qualitative Methods, 22. https://doi.org/10.1177/16094069231205789
Naranjee, N., Ngxongo, T. S. P., & Sibiya, M. N. (2019). African Journal of Primary Health Care & Family Medicine. Afr J Prm Health Care Fam Med, 11(1), 1981. https://doi.org/10.4102/phcfm
Oxford Academic. (2024). Consolidated criteria for reporting qualitative research (COREQ)_ a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. https://academic.oup.com/intqhc/article/19/6/349/1791966
Polit, D. F., & Beck, C. T. (2018). Nursing Research: Generating and Assessing Evidence for Nursing Practice. Wolters Kluwer Health/lippincott Williams & Wilkins. https://books.google.com.et/books?id=Ej3wstotgkQC
Powers, K., Pate, K., Montegrico, J., & Pagel, J. (2022). Faculty Perceptions of the Impact of the COVID-19 Pandemic on New Graduate Nurses’ Transition to Practice: A Qualitative Study. Journal of Professional Nursing, 43, 33–41. https://doi.org/10.1016/j.profnurs.2022.09.003
Rush, K. L., Janke, R., Duchscher, J. E., Phillips, R., & Kaur, S. (2019). Best practices of formal new graduate transition programs: An integrative review. In International Journal of Nursing Studies (Vol. 94, pp. 139–158). Elsevier Ltd. https://doi.org/10.1016/j.ijnurstu.2019.02.010
Saifan, A., Devadas, B., Daradkeh, F., Abdel-Fattah, H., Aljabery, M., & Michael, L. M. (2021). Solutions to bridge the theory-practice gap in nursing education in the UAE: a qualitative study. BMC Medical Education, 21(1). https://doi.org/10.1186/s12909-021-02919-x
Salifu, D. A., Gross, J., Salifu, M. A., & Ninnoni, J. P. K. (2019). Experiences and perceptions of the theory-practice gap in nursing in a resource-constrained setting: A qualitative description study. Nursing Open, 6(1), 72–83. https://doi.org/10.1002/nop2.188
Sriram, V., Brophy, S. A., Sharma, K., Elias, M. A., & Mishra, A. (2023). Associations, unions and everything in between: contextualising the role of representative health worker organisations in policy. BMJ Global Health, 8(9). https://doi.org/10.1136/bmjgh-2023-012661
Stavropoulou, A., Rovithis, M., Kelesi, M., Vasilopoulos, G., Sigala, E., Papageorgiou, D., Moudatsou, M., & Koukouli, S. (2022). What Quality of Care Means? Exploring Clinical Nurses’ Perceptions on the Concept of Quality Care: A Qualitative Study. Clinics and Practice, 12(4), 468–481. https://doi.org/10.3390/clinpract12040051
Voldbjerg, S. L., Nielsen, G. N., Klit, M. O., Larsen, K. L., & Laugesen, B. (2022). Clinical supervisors’ perceptions and use of the fundamentals of care framework in supervision of nursing students. Journal of Advanced Nursing, 78(12), 4199–4209. https://doi.org/10.1111/jan.15408
Vosoughi, M. N., Zamanzadeh, V., Valizadeh, L., Ghahramanian, A., Lotfi, M., Bagheriyeh, F., & Pourmollamirza, A. (2022). An introduction to the TPSN model: a comprehensive approach to reducing the theory-practice gap in nursing. BMC Nursing, 21(1). https://doi.org/10.1186/s12912-022-01030-w
WHO. (2018). Handbook for national quality policy and strategy: a practical approach for developing policy and strategy to improve quality of care. WHO. http://apps.who.int/bookorders.
WHO. (2020). STATE OF THE WORLD’S NURSING 2020: Investing in education, jobs and leadership. World Health Organization.
WHO. (2021). GLOBAL PATIENT SAFETY ACTION PLAN 2021–2030: Towards eliminating avoidable harm in health care.
WHO. (2023). Patient safety. https://www.who.int/news-room/fact-sheets/detail/patient-safety
Willman, A., Bjuresäter, K., & Nilsson, J. (2020). Newly graduated registered nurses’ self-assessed clinical competence and their need for further training. Nursing Open, 7(3), 720–730. https://doi.org/10.1002/nop2.443
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Jurnal Ners dan Kebidanan (Journal of Ners and Midwifery)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.


 University of South Africa, Pretoria, South Africa
University of South Africa, Pretoria, South Africa Google Scholar
Google Scholar ORCID
ORCID Scopus
Scopus



