Integration Telemental Health to Reach Out Patients at Community Mental Health Services: A Systematic Review
DOI:
https://doi.org/10.26699/jnk.v11i2.ART.p189-199Keywords:
telemental health, mobile health, telepsychiatry, mental health servicesAbstract
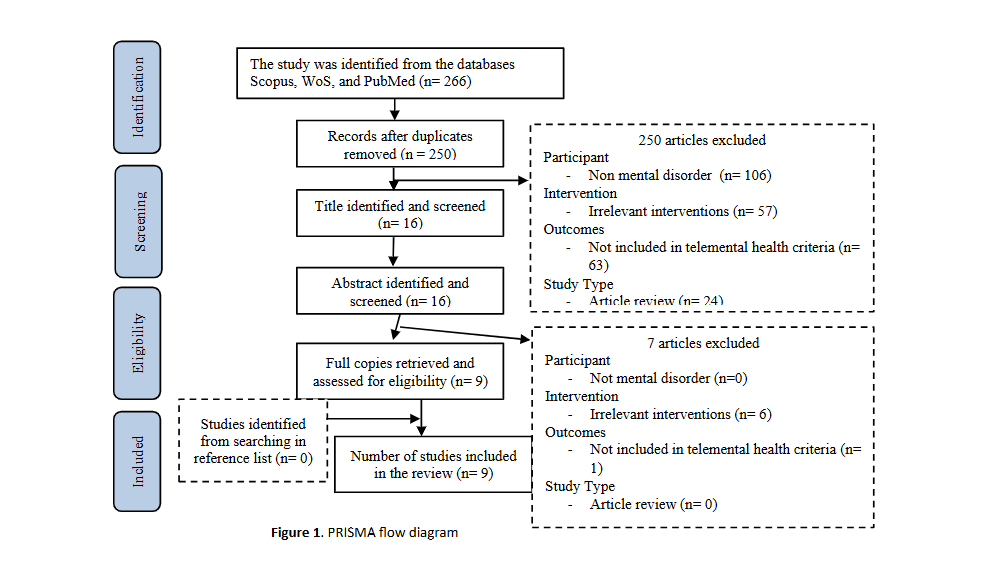
Low- and middle-income countries (LMICs) need to digitize mental health services to address disparities and improve access to healthcare. This study systematically reviewed the digitalization of integration mental health services that can reach interactions between service providers and recipients with media such as telemental health and mobile health. A literature search was conducted in March 2023. Randomized controlled trial (RCT) data were used from available studies. RCT data sources were obtained from internationally reputable journal articles with the theme of telehealth. The literature used was obtained from the databases Scopus, Web of Science, and PubMed. Integration digitalized mental healthcare system under the auspices of the Ministry of Health that reach-nationally, official psychiatrists and other professional mental healthcare that provides mental healthcare support to areas lacking specialists consisting crisis and emergency, stable conditions, as well as the process of counseling and follow-up therapy with telemental health and mobile health media. Telemental health plays a major role in mental health services and modality therapy that can be accessed effectively and efficiently, especially for mental patients in remote areas who experience barriers to attending in person.
References
Adem, J. B., Zeleke, T., Walle, A. D., Atinafu, W. T., Tilahun, K. N., Melaku, M. S., & Kebede, S. D. (2023). Awareness and readiness of mental healthcare providers to implement telemental health services and associated factors at public referral hospitals in Addis Ababa City, Ethiopia. BMJ Open, 13(7), 1–13. https://doi.org/10.1136/bmjopen-2022-069671
Ben-Zeev, D., Buck, B., Hallgren, K., & Drake, R. E. (2019). Effect of mobile health on in-person service use among people with serious mental illness. Psychiatric Services, 70(6), 507–510. https://doi.org/10.1176/appi.ps.201800542
Ben-Zeev, D., Chander, A., Tauscher, J., Buck, B., Nepal, S., Campbell, A., & Doron, G. (2021). A smartphone intervention for people with serious mental illness: Fully remote randomized controlled trial of CORE. Journal of Medical Internet Research, 23(11). https://doi.org/10.2196/29201
Bendtsen, M., Müssener, U., Linderoth, C., & Thomas, K. (2020). A mobile health intervention for mental health promotion among university students: Randomized controlled trial. JMIR MHealth and UHealth, 8(3). https://doi.org/10.2196/17208
Bunnell, B. E., Barrera, J. F., Paige, S. R., Turner, D., & Welch, B. M. (2020). Acceptability of telemedicine features to promote its uptake in practice: a survey of community telemental health providers. International Journal of Environmental Research and Public Health, 17(22), 1–15. https://doi.org/10.3390/ijerph17228525
Chaudhry, S., Weiss, A., Dillon, G., O’Shea, A., & Hansel, T. C. (2022). Psychosis, Telehealth, and COVID-19: Successes and Lessons Learned from the First Wave of the Pandemic. Disaster Medicine and Public Health Preparedness, 16(5), 1785–1788. https://doi.org/10.1017/dmp.2021.42
De Sousa, A., Mohandas, E., & Javed, A. (2020). Psychological interventions during COVID-19: Challenges for low and middle income countries. Asian Journal of Psychiatry, 51. https://doi.org/10.1016/j.ajp.2020.102128
Dursun, O. B., Turan, B., Pakyürek, M., & Tekin, A. (2021). Integrating Telepsychiatric Services into the Conventional Systems for Psychiatric Support to Health Care Workers and Their Children during COVID-19 Pandemics: Results from A National Experience. Telemedicine and E-Health, 27(3), 269–275. https://doi.org/10.1089/tmj.2020.0237
Elugbadebo, O. O., Ojagbemi, A. A., & Gureje, O. (2023). Mobile phone intervention to reduce dropout from treatment at an outpatient mental health service for older people in Nigeria. African Health Sciences, 23(4), 551–562. https://doi.org/10.4314/ahs.v23i4.58
Graham, A. K., Greene, C. J., Kwasny, M. J., Kaiser, S. M., Lieponis, P., Powell, T., & Mohr, D. C. (2020). Coached mobile app platform for the treatment of depression and anxiety among primary care patients: A randomized clinical trial. JAMA Psychiatry, 77(9), 906–914. https://doi.org/10.1001/jamapsychiatry.2020.1011
Jannati, N., Yazdi-Feyzabadi, V., Sarabi, R. E., & Salehinejad, S. (2021). How to deal with the mental health consequences of global health emergencies? A nutshell of telemental health services and its requirements. Journal of Emergency Practice and Trauma, 7(2), 127–129. https://doi.org/10.34172/jept.2021.14
Lawson, J. L., Doran, J. M., O’Shea, M. K., & Abel, E. A. (2022). The Good, The Bad, The Uncertain: Diverse Provider Experiences with Telemental Health During COVID-19. Psychiatric Quarterly, 93(3), 753–774. https://doi.org/10.1007/s11126-022-09990-7
Lewis, S., Ainsworth, J., Sanders, C., Stockton-Powdrell, C., Machin, M., Whelan, P., Hopkins, R., He, Z., Applegate, E., Drake, R., Bamford, C., Roberts, C., & Wykes, T. (2020). Smartphone-enhanced symptom management in psychosis: Open, randomized controlled trial. Journal of Medical Internet Research, 22(8). https://doi.org/10.2196/17019
Mohr, D. C., Tomasino, K. N., Lattie, E. G., Palac, H. L., Kwasny, M. J., Weingardt, K., Karr, C. J., Kaiser, S. M., Rossom, R. C., Bardsley, L. R., Caccamo, L., Stiles-Shields, C., & Schueller, S. M. (2017). IntelliCare: An Eclectic, Skills-Based App Suite for the Treatment of Depression and Anxiety. J Med Internet Res, 19(1), e10. https://doi.org/10.2196/jmir.6645
Moitra, E., Park, H. S., & Gaudiano, B. A. (2021). Development and Initial Testing of an mHealth Transitions of Care Intervention for Adults with Schizophrenia-Spectrum Disorders Immediately Following a Psychiatric Hospitalization. Psychiatric Quarterly, 92(1), 259–272. https://doi.org/10.1007/s11126-020-09792-9
Ricklan, S. J., Sohler, N., Ezie, C. E. C., Avalone, L., Dinsell, V., Lewis, C., Fattal, O., Balan, S., McQuistion, H., Pastore, F., Sarcevic, N., Swift, R., Espejo, G., & Lorenz, C. (2024). Impact of Telemedicine on Utilization of Psychiatric Resources in New York City during the COVID-19 Pandemic. Community Mental Health Journal, 60(1), 115–123. https://doi.org/10.1007/s10597-023-01210-1
Röhricht, F., Padmanabhan, R., Binfield, P., Mavji, D., & Barlow, S. (2021). Simple Mobile technology health management tool for people with severe mental illness: a randomised controlled feasibility trial. BMC Psychiatry, 21(1). https://doi.org/10.1186/s12888-021-03359-z
Shang, Z., Arnaert, A., Hindle, Y., Debe, Z., Côté-Leblanc, G., & Saadi, A. (2021). Experiences of psychiatrists and support staff providing telemental health services to Indigenous peoples of Northern Quebec. BMC Health Services Research, 21(1). https://doi.org/10.1186/s12913-021-06072-5
Sreejith, G., & Menon, V. (2019). Mobile Phones as a Medium of Mental Health Care Service Delivery: Perspectives and Barriers among Patients with Severe Mental Illness. www.ijpm.info. https://doi.org/10.4103/IJPSYM.IJPSYM_333_18
Weissinger, A. C., Burns, R., & Campbell, N. J. (2021). Evaluating Emergency Department Utilization for Mobile Mental Health Patients: A Correlational Retrospective Analysis. Journal of the American Psychiatric Nurses Association, 27(5), 383–389. https://doi.org/10.1177/1078390320916236
Wilczewski, H., Paige, S. R., Ong, T., Soni, H., Barrera, J. F., Welch, B. M., & Bunnell, B. E. (2022). Providers’ Perspectives on Telemental Health Usage After the COVID-19 Pandemic: Retrospective Analysis. JMIR Formative Research, 6(11). https://doi.org/10.2196/39634
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Jurnal Ners dan Kebidanan (Journal of Ners and Midwifery)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.




 Google Scholar
Google Scholar Research Gate
Research Gate Sinta
Sinta
 Google Scholar
Google Scholar Research Gate
Research Gate One Research
One Research ORCID
ORCID